 Patellar tendonitis is a deceitful injury. It will trick you into letting it weaken your knees until you’ll eventually need months of rehab.
Patellar tendonitis is a deceitful injury. It will trick you into letting it weaken your knees until you’ll eventually need months of rehab.
This article will show you the symptoms of patellar tendonitis and the three red flags that tell you how serious your patellar tendonitis has become.
Keep reading to learn how you can get rid of patellar tendonitis symptoms and stop this injury dead in its tracks.
Before continuing, read the full disclaimer here.
Patellar Tendonitis Symptoms: Where You Will Feel the Pain
The patellar tendon connects your patella, the kneecap, to the shinbone. You use this tendon every time you straighten your knee.
This tendon can withstand very high forces, but in spite of its durability, the patellar tendon can still wear down over time if it’s frequently overstressed.
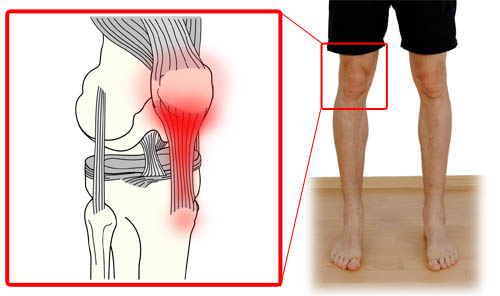
With patellar tendonitis, the pain will be located around the patellar tendon. You will feel it on the side of your kneecap, in front of your kneecap, and sometimes even behind the kneecap. Most commonly, the pain is felt in the patellar tendon right below the kneecap.
Some symptoms that don’t happen with patellar tendonitis are pain on the side of the knee, pain behind the knee, swelling of the knee, or inability to fully flex or extend the knee.
Activities That Worsen the Symptoms
You use the patellar tendon every time you extend your knee. All activities that involve this movement can worsen the pain. This includes climbing stairs, squatting, cycling, and walking downhill.
Explosive leg movements, such as jogging, weightlifting, jumping, and sprinting are particularly likely to worsen the pain.
Patellar Tndonitis Stages
Research shows that the further you let your patellar tendonitis progress, the more cellular damage will have occurred in your tendon and the weaker it will have become. The weaker the tendon becomes the more of its resilience you’ll lose.
The longer you wait, the weaker your knee becomes and the more recovery time you’ll ultimately need.
This means that activities that didn’t cause you pain when you’re in stage 1 of patellar tendonitis are too stressful for your knee when you’re in stage 2 or 3 and will then cause pain.
Additionally, based on what stage you’re in, the injury requires a different healing approach. With that in mind you can understand why it’s very important to know about the symptoms for the individual stages of patellar tendonitis.
Each stage has one red flag symptom that indicates your injury has progressed to this stage.
Here’s an overview of these stages and their red flag symptoms:
Stage 1 Symptoms
- No symptoms during sports activity
- Light ache to mild pain after activity
- Symptoms disappear within a day
Stage 2 Symptoms
- Light ache during sports activity
- Mild pain after the activity
- You’ve had pain some time ago and it went away, but now it’s back
Red flag symptom: Pain lingers for more than two days and keeps coming back after activity.
Stage 3 Symptoms
This is where most people realize that they need to do something about it.
- Mild pain before sports activity
- Pain during activity
- Moderate to strong pain after activity
Red Flag: Pain starts to limit sports performance and there is always some pain throughout the day, even after a lot of rest.
Stage 4 Symptoms
At this stage, the risk of tearing your patellar tendon has become very high. Pain strongly impairs sports performance and everyday activities have become very painful
Please note: this does not replace a thorough examination by your doctor! This list is merely meant to give you an idea of how far your injury has already progressed.
The 2 Types of Healing Requirements
There are two types of healing requirements for patellar tendonitis you need to know if you want to get back to being 100% healthy. They dictate which approach to healing you need to take and depend on which stage of the injury you’re in.
One healing requirement both have in common is that you need to eliminate hidden biomechanical causes for your patellar tendonitis or else it will come back like clockwork [for biomech. risk factors, see for example (Backman, Danielson 2011), (Powers 2010), (Grau et al. 2008), or (Ireland et al. 2003)].
Here is the first set of requirements:
Healing Requirements for Stage 1:
- Rest until pain is gone
- Improve biomechanics to reduce load on patellar tendon
(Patellar tendonitis symptoms will ALWAYS RETURN if you don’t do this!) - Reduce training load to prevent return of pain
During the research for my book, I’ve discovered that the only stage in which resting will lead to complete healing is stage #1. In other words, if you have any of the red flag symptoms for stages two through four, resting will not get you back to 100%.
The second set of requirements applies to the chronic stages of patellar tendonitis, when the symptoms have become somewhat constant:
Healing Requirements for Stages 2 – 4:
- Resting will not heal your tendon completely, you need to…
- Use specific healing exercises to repair the patellar tendon
(e.g., safe isometric and eccentric exercises) (Larsson et al. 2012, p. 1643) - Improve biomechanics to reduce load on patellar tendon
- Track your pain levels and modify your training to reduce pain over time
- Optimize your diet to improve tendon healing through increased collagen formation
Your Next Steps
When I had patellar tendonitis, I waited much too long before doing something about. I made that mistake because I thought patellar tendonitis would go away on its own, but it only became worse.
Academic research shows that chronic patellar tendonitis will not go away on its own. You need to do the right things for the stage of the injury you’re in or else you risk months of rehab and no sports, as well constant pain. (Cook, Purdam 2009, p. 409ff)
I want to prevent this from happening to you, but you need to take action. Here’s your best option.
Citations and Further Reading
Backman, Ludvig J.; Danielson, Patrik (2011): Low range of ankle dorsiflexion predisposes for patellar tendinopathy in junior elite basketball players: a 1-year prospective study. In Am J Sports Med 39 (12), pp. 2626–2633. DOI: 10.1177/0363546511420552.
Cook, J. L.; Purdam, C. R. (2009): Is tendon pathology a continuum? A pathology model to explain the clinical presentation of load-induced tendinopathy. In British Journal of Sports Medicine 43 (6), pp. 409–416. DOI: 10.1136/bjsm.2008.051193.
Grau, S.; Maiwald, C.; Krauss, I.; Axmann, D.; Janssen, P.; Horstmann, T. (2008): What are causes and treatment strategies for patellar-tendinopathy in female runners? In J Biomech 41 (9), pp. 2042–2046. DOI: 10.1016/j.jbiomech.2008.03.005.
Ireland, Mary Lloyd; Willson, John D.; Ballantyne, Bryon T.; Davis, Irene McClay (2003): Hip strength in females with and without patellofemoral pain. In J Orthop Sports Phys Ther 33 (11), pp. 671–676.
Larsson, Maria E. H.; Käll, Ingela; Nilsson-Helander, Katarina (2012): Treatment of patellar tendinopathy—a systematic review of randomized controlled trials. In Knee Surg Sports Traumatol Arthrosc 20 (8), pp. 1632–1646. DOI: 10.1007/s00167-011-1825-1.
Powers, Christopher M. (2010): The influence of abnormal hip mechanics on knee injury: a biomechanical perspective. In J Orthop Sports Phys Ther 40 (2), pp. 42–51. DOI: 10.2519/jospt.2010.3337.
Photo Credit
Joe Christiansen on Flickr (https://www.flickr.com/photos/joe_milkman/5190409637/in/photostream/)
