What are the most time-effective exercises to get rid of knee pain?
How can you ensure fast training progress by staying injury-free?
For this article, I turned to academic research to find the answer.
First, I investigated biomechanical causes of the most common leg injuries: knee pain, ankle sprains, and plantar fasciitis.
Then I took an exhaustive list of corrective exercises to improve these biomechanical factors and distilled it down to the most potent drills.
Here’s what you will find on this page:
- The Infographic: Everything you need to know compressed into one image
- The Science: A short explanation of the risk factors and the exercises
- The Training Plan: A minimalist corrective routine for your workouts
The Infographic: How to Make Leg Injuries History
“Everything should be made as simple as possible, but no simpler.” – Einstein[1]
I compressed everything you need to know into the following infographic. It offers a minimalist approach to preventing leg injuries and many of my readers have used these exercises to get rid of knee pain.
For your safety, I strongly recommend you work with a qualified medical expert if you are injured, or suspect that you have an injury. The following exercises only form the foundation of a good rehab program, but depending on your individual situation, you may need additional (or different) exercises.
Share This Image on Your Site:
This infographic cost me a month of research and over 2000 EURO in designer fees.
Please leave the links intact 🙂
Using Better Science to Build Healthy Legs (And Get Rid of Knee Pain)
The most common leg injuries are knee pain (10.4 Million per year[2]), ankle injuries (2 Million per year[3]), and plantar fasciitis (1 Million per year[4]). Behind these statistics are men, women, and children that suffer great emotional pain and financial pressure.
In 2011, Fix-Knee-Pain.com was born from my desire to help people with knee pain get back to enjoying their lives, by providing a comprehensible and applicable system of what science and the smartest physicians of our time have discovered about injury prevention and rehab.
After all, what’s the point of having 2.5 Million research papers published each year[5], if almost nothing of it finds practical application?
To determine the exercises best suited for preventing leg injuries, we have to examine their most common risk factors. Let’s start with knee pain.
Knee Pain Risk Factors
Many smart thinkers have written about why these risk factors cause or contribute to knee pain, so if you want to learn details about individual items on these lists, I highly recommend you read the linked articles or check out the references at the bottom of this page.
I intentionally selected the exercises in the 5-step plan of the infographic based on how well they can help you fix these knee pain causes. Here’s the first risk factor.
1) Previous Knee Injury [6],[7],[8],[9],[10],[11]
Statistically, having suffered a knee injury in the past dramatically increases your odds of getting knee pain again in the future. However, based on my experience, I’m convinced this has a lot to do with insufficient work on the actual causes of pain in favor of a treatment approach focused on eliminating pain itself quickly (i.e., symptom treatment).
In other words, even if you had pain in the past you can still get better if you work on the following knee pain causes.
2) Low Mobility or Stability at the Hip or Ankle [12],[13],[14],[15],[16],[17],[18],[19],[20]
The knee is a slave to what happens at the ankle and the hip. This topic actually deserves a much closer examination, but we’ll focus on two key aspects for the sake of brevity: mobility and stability.
Mobility is about what a joint system can do without external force. Stability is the ability of a joint system to maintain its position in the presence of an external force. Put simply, mobility allows for movement, whereas stability controls movement.
Each major joint system requires one aspect’s dominance, as illustrated by the following picture.
Here’s why this matters.
If you lack mobility at the hip or the ankle, the body will make up for it by increasing mobility demands on the neighboring joints – the knee and the lower back – forcing them to “work overtime”. Eventually, the knee and the lower back become overused and painful.
However, problems also arise if you lack stability at the hip or in other words, if you cannot control hip position in the presence of an external force (see cause #4 below). This external force could just be gravity, but it could also be much higher, for example during the acceleration and deceleration when running and jumping.
Academic research has confirmed how important strong and flexible hips, as well healthy ankles are for preventing knee pain. If you want to learn more about this fascinating topic, check out the Joint-by-Joint Approach by Dr. Gray Cook and Michael Boyle, as well as their expanded version.
3) Tightness in the Quads, Hip Flexors, Hamstrings, or Calves [21],[22],[23]
Tightness in any of these four muscles can contribute to knee pain, mostly because they introduce excessive tension to the knee. They’re also indicative of a movement dysfunction.
The most common movement dysfunction of our time is the result of too much sitting. This leads to certain muscles getting weak, like the gluteal muscles on the side and back of your hip, with others getting “tight”, like the hip flexors on the front of your hip.
Movement dysfunction eventually overworks certain body parts. The result may just be a tight muscle, like a tight hamstring, but it could also be an injury, like knee pain, plantar fasciitis, or a torn hamstring.
The dysfunction will spread from one place in your body to another, which is why examining the body as a whole is so critically important. Conservative medicine falls short by only looking at the site of pain and while that’s great for treating acute injuries like a fracture, it won’t help you with chronic issues.
4) Low Skill at Single-Leg Exercises & Bad Leg Alignment [24],[25],[26],[27],[28],[29],[30]
How well you can keep your legs aligned when you’re moving on one foot determines how much excessive stress you’re placing on certain tissues of your knee.
For example, if your knee collapses towards the midline of your body, you’re putting your patellar tendon, your ACL, and your Achilles tendon under abnormal load. That’s why alignment problems contribute to overuse injuries in those tissues.
If you do this fast enough on one leg, your ACL may need surgery.
To prevent bad alignment, you first have to strengthen and mobilize your hips. Then you need to “update” your motor control center by paying attention to correct alignment during your day and as you’re doing sports.
Single-leg exercises, like the hip hinge progression in step 4 of the infographic, will help you become aware of problems in this area. Additionally, they will make the strength you built with isolated hip strengthening exercises (step 3) carry over into real-world applications by improving your hip stability.
5) Wait, there’s more! Other Knee Pain Risk Factors
Other knee pain risk factors include doing sports that require strong quads for optimal performance[31], a high training volume[32], over-pronation[33], being overweight[34], and having inflammation in your body[35]. Weak quadriceps muscles also put you at risk[36].
A lot more could be written about each of these topics, but I want to be respectful of your time, so let me finish with this surprising fact.
I was fascinated when I discovered that in patellar tendonitis (“Jumper’s Knee”), tissue damage occurs before you feel pain[37] and I suspect the same applies to other types of knee injuries as well.
In other words, once you feel something in your knee, the damage has already been done. At that point, you’re left with two options.
You could continue your regular training and watch your rehab efforts fail[38] or you could make healing your priority and get well. Most people only prioritize rehab once their pain leaves them no other choice and that’s unfortunate, because the longer you ignore pain, the worse it becomes and the longer it will ultimately take to heal.
Plantar Fasciitis Risk Factors
As you’ll see in a moment, the risk factors for knee pain and for plantar fasciitis share some similarities. That’s why the exercises in the infographic can help you with both problems at the same time.
Each year, around 300 Million dollars are spent on physician visits and treatments for plantar fasciitis[39]. In one study, 70% of people with plantar fasciitis were found to be obese[40] and other studies confirmed obesity as a risk factor[41], but there’s more to it.
Obesity was only associated with higher risk in non-athletic patients! More interesting yet, while obesity elevated risk overall 2.4-times, tight hamstrings lead to an impressive 8.7-times increase[42]. Tight calves and ankles also put you at risk[43],[44] with low ankle dorsiflexion being present in 53% of patients[45].
Over-pronation occurred in 81% of patients[46] and flat feet are another risk factor[47]. However, using orthotics only provided a very small benefit at the 3-month follow-up, with no long-term benefit at the 12-month interval[48].
The challenge with plantar fasciitis is that walking and standing on hard surfaces also increases risk[49], but we can’t just sit around all day.
One Shoe Problem That Contributes to Pain
Some people with plantar fasciitis found that wearing healthier shoes also helped them get better. For example, one potentially problematic shoe feature is the toe spring or toe lift.

This toe lift places the plantar fascia under permanent tension by lifting the toes up. I only had a dress shoe to illustrate it, but the toe lift can be much higher in sport’s shoes, thereby causing more tension in the plantar fascia.
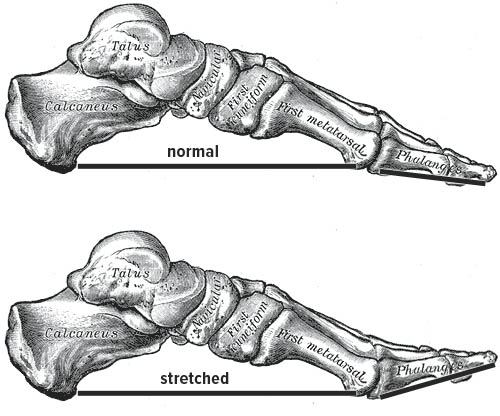
The basic treatment approach for plantar fasciitis is to wear shoes with a flat sole and no toe lift in addition to stretching your calves and your hamstrings.
For a more detailed examination of plantar fasciitis, please read physical therapist James Speck’s articles on the real cause of plantar fasciitis, why conventional treatments are prone to failure, and his ultimate guide on plantar fasciitis.
More Surprises: Here’s What Really Causes Ankle Injuries
One study on ankle injuries found that athletes with a BMI higher than 23.1 had 8-fold greater odds of suffering an ankle sprain[50] (calculate your BMI here).
For comparison, if you’ve suffered an ankle injury in the past, you’re at a 4.9-times greater risk[51], but get this, if you wear shoes with air cells in their heels, your risk also increases 4.3-times!
Shoes with air cells put athletes at a significantly greater risk of injuring their ankle[52], even though the protective response in the lower leg muscles also increases when wearing shoes with thick soles[53].
Howard Hillstrom, PhD, director of the Leon Root Motion Analysis Laboratory at the Hospital for Special Surgery in New York City, pointed out that spraining your ankle is difficult if you’re barefoot. He explained that by wearing shoes, you’re reducing the freedom of articulation in your feet and introducing an artificial point of instability “… due to the edge of the shoe under the lateral aspect of the foot.”[54]
My own explanation of the mechanism of injury is that sole thickness increases the lever arm between your ankle joint and the ground, which means your lower leg muscles have to work harder to oppose forces that would otherwise cause a sprain.
How Strong Are Your Lower Leg Muscles?
Several studies support the importance of strong lower leg muscles.
A 2012 prospective study on professional soccer players found asymmetries in ankle flexion strength to increase odds of ankle injury 8.88-times[55], which is even more than being overweight! In those that suffered a past ankle injury, a “neuromuscular deficit” could contribute to these asymmetries[56].
Other muscular problems associated with ankle instability are weakness in peroneal muscles, ankle dorsiflexors, and hip abductors[57],[58]. Additionally, weak single-leg balance is a risk factor for leg injuries[59] and it may increase odds for ankle injuries as much as 7-fold[60].
Good News Everyone
A large body of evidence supports the positive therapeutic effects of balance training[61]. For example, a 6-year study on professional basketball players found that proprioceptive training reduced occurrence of ankle sprains by 81%[62].
Beyond balance training, another research team discovered that practicing proper landing technique reduced occurrence of ankle injuries by 45%[63]. Ankle taping can also be very useful when applied properly.
My conclusion on ankle sprains is that we can reduce risk dramatically by doing balance training on solid ground, by improving ankle and hip mobility, by strengthening hip muscles, and by wearing shoes with a thin sole. Unfortunately, the choice of footwear strongly depends on your sport and your body’s preparedness for thin-soled shoes. s
Explaining the 5-Step System to Get Rid of Knee and Build Healthy Legs
So far, you’ve gone through a crash-course on the actual causes of knee pain, plantar fasciitis, and ankle injuries. A lot more could be said about each individual injury, but by now we know enough to come up with a science-based training plan for healthy legs. First, here’s why I prefer training to surgery.
In their article on risk of surgery, the Scientific American writes that anesthesia drugs “… bind to and incapacitate several different proteins on the surface of neurons that are essential for regulating sleep, attention, learning, and memory.”
Call me old-fashioned, but these are things I’d rather leave alone if possible, especially if the mechanism of action is so little understood: “[I]t seems that interrupting the usual activity of neurons may disrupt communication between far-flung regions of the brain, which somehow triggers unconsciousness.”
I’m not comfortable with that level of uncertainty. We should at least expect good rewards taking such high risks, but that may not be the case. In acute injuries (i.e., fractures, bleeding, torn cartilage or ligaments etc.) caused by accidents, surgery is the best option, but what about chronic injuries?
The research I read for my book Beating Patellar Tendonitis concluded that surgery provided inconsistent outcomes[64], while other researchers found that the strongest evidence only existed for physical training[65]. I suspect that a similar situation exists for other chronic leg injuries, making exercise by far the preferable first choice in terms of the risk-reward-ratio.
Let me explain how each of the 5-steps in the training plan addresses the actual causes we discovered earlier.
Step 1: Self-Massage
I first discovered self-massage through Mike Robertson and Eric Cressey. Here’s what self-massage will do for you.
- Help correct muscular imbalances by releasing soft-tissue restrictions.
- Increase flexibility and hip mobility.
- Help injuries heal faster by releasing tension from your legs.
- Improve your posture.
- Allow better athletic performance.
- Reduce muscle tightness safely.
Professional treatment from a qualified practitioner can provide faster results, but with regular maintenance through self-massage, this may not become necessary.
Step 2: Hip Flexor Stretches
Credit for the couch stretch goes to Dr. Kelly Starrett. These two stretches will counter the negative effects of sitting by releasing tension from your hip flexors, which is required for optimal hip mobility and stability.
The hips are tremendously important for healthy legs and a healthy lower back. That’s what we’re working on them with the following step as well.
Step 3: Gluteal Strengthening Exercises
I admit they’re not particularly exciting, but these three drills are crucial for the following reasons.
- Strengthen hip muscles that stabilize the knee.
- Reduce risk of ankle injuries and over-pronation.
- Release tightness from overworked hamstrings, by strengthening their synergists.
- Make you look better.
- You will jump higher and run faster, once your body knows how to use these muscles well.
Academic research supports the benefit of hip strengthening exercises, especially when used in conjunction with stretches [66],[67],[68],[69],[70],[71],[72],[73].
Step 4: The Hip Hinge Progression
The one-legged deadlift is a true jack-of-all-trades type of exercise. Done correctly, it will give you a myriad of benefits, which is why the return on time invested is spectacular. Here are two caveats.
First, you will be tempted to skip the stick variations because they’re “easy” and because you may be too lazy to go to your broom closet and grab a stick. Don’t make that mistake. Practice technique with the stick for a few hundred repetitions before you move on to using weights.
The second caveat is that it’s tempting to use too much weight too quickly, which erodes exercise technique and puts your back and your legs at risk of injury. As an analogy, you wouldn’t let a teenager drive a 400 Horsepower car on the highway during his very first driving lesson.
Be smart with your body and the one-legged deadlift will give you the following benefits.
- Strengthen your upper and lower back.
- Help relieve back pain by teaching good back alignment during weight-bearing exercises.
- Strengthen your hamstrings, gluteal muscles, and grip.
- Reduce risk of ankle sprains by strengthening the lower leg muscles.
- Make you look better.
- Prevent ACL-tears by teaching you to avoid bad leg alignment.
- Allows you to use the hip muscles we strengthened in step 3 in real-world scenarios.
- Improve posture.
- Allow knee pain to heal faster by reducing forward knee movement and teaching the hip hinge.
- Improve hip stability.
Practicing this exercise helped me avoid two possibly serious ankle sprains in basketball.
Both times, I landed on another player’s foot, but my lower leg muscles were strong enough to compensate for the uneven ground, thereby preventing the sprain. In one case, I didn’t even notice it until the guy started screaming at me to get off his foot.
Step 5: A Pinch of Ankle Mobility
Lack of ankle mobility, specifically dorsiflexion, turned out to be a risk factor for all three injuries, which is why we’re working on it with the dorsiflexion drill. If you have knee pain, you can make this exercise easier on your knee by placing a book under the balls of your feet and doing it standing.
The samurai sit, on the other hand, will stretch your toes and help improve big toe mobility. A restricted big toe can cause knee pain and back pain, because it influences how your whole body moves during gait. Be careful with the samurai sit if you have plantar fasciitis, as it will stretch the plantar fascia, which could increase pain.
Before I end this article, here’s why some people could criticize this approach.
Criticism: Correlation vs. Causation
Most of the research I cited in this article doesn’t talk about “causes,” but rather about odds-ratios, p-values, and other statistical terms. I understand that correlation does not equal causation, but until we have better data, we need to rely on the old scientific approach of making a hypothesis and then testing it.
The exercises I shared above have indeed been shown to be very potent in the work of rehab professionals. My own experience in helping people get rid of knee pain confirms this as well, but as I said in the introduction, they’re only the foundation of a good rehab program, since everyone has slightly different needs that may necessitate additional exercises.
Your Next Steps
Did you find this useful? Let me know by sharing this material on your website, on Facebook, or by sending emails to three friends that could benefit. I depend on your help to reach as many people as possible.
Next, if you have knee pain, I will help you get back to enjoying your life by sharing some of my most effective techniques in my advanced course on getting rid of knee pain. Over 21,000 people have taken the course since I offered the first version in 2011.
Finally, download your short training routine to start building unbreakable legs to day.
References
[1] Garson O’Toole, “Everything Should Be Made as Simple as Possible, But Not Simpler,” accessed March 7, 2016, http://quoteinvestigator.com/2011/05/13/einstein-simple/
[2] “Common Knee Injuries,” American Academy of Orthopedic Surgeons, accessed March 8, 2016, http://orthoinfo.aaos.org/topic.cfm?topic=a00325
[3] Douglas Ivins, “Acute Ankle Sprain: An Update,” American Academy of Family Physicians, accessed March 8, 2016, http://www.aafp.org/afp/2006/1115/p1714.html
[4] James D. Goff, “Diagnosis and Treatment of Plantar Fasciitis,” American Academy of Family Physicians, accessed March 8, 2016, http://www.aafp.org/afp/2011/0915/p676.html
[5] Sarah Boon, “21st Century Science Overload,” Canadian Science Publishin, accessed March 8, 2016, http://www.cdnsciencepub.com/blog/21st-century-science-overload.aspx
[6] Behzad Heidari, “Knee osteoarthritis prevalence, risk factors, pathogenesis and features: Part I,” Caspian journal of internal medicine 2, no. 2 (2011)
[7] V. Silverwood et al., “Current evidence on risk factors for knee osteoarthritis in older adults: a systematic review and meta-analysis,” Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society 23, no. 4 (2015), doi:10.1016/j.joca.2014.11.019
[8] H. Miranda et al., “A prospective study on knee pain and its risk factors,” Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society 10, no. 8 (2002)
[9] C. Cooper et al., “Risk factors for the incidence and progression of radiographic knee osteoarthritis,” Arthritis and rheumatism 43, no. 5 (2000), doi:10.1002/1529-0131(200005)43:5<995::AID-ANR6>3.0.CO;2-1
[10] Shigeyuki Muraki et al., “Incidence and risk factors for radiographic knee osteoarthritis and knee pain in Japanese men and women: a longitudinal population-based cohort study,” Arthritis and rheumatism 64, no. 5 (2012), doi:10.1002/art.33508
[11] B. Marti et al., “On the epidemiology of running injuries. The 1984 Bern Grand-Prix study,” The American journal of sports medicine 16, no. 3 (1988)
[12] Mary L. Ireland et al., “Hip strength in females with and without patellofemoral pain,” The Journal of orthopaedic and sports physical therapy 33, no. 11 (2003)
[13] Christopher M. Powers, “The influence of abnormal hip mechanics on knee injury: a biomechanical perspective,” The Journal of orthopaedic and sports physical therapy 40, no. 2 (2010), doi:10.2519/jospt.2010.3337
[14] Ludvig J. Backman and Patrik Danielson, “Low range of ankle dorsiflexion predisposes for patellar tendinopathy in junior elite basketball players: a 1-year prospective study,” The American journal of sports medicine 39, no. 12 (2011), doi:10.1177/0363546511420552
[15] Peter Malliaras, Jillianne L. Cook, and Peter Kent, “Reduced ankle dorsiflexion range may increase the risk of patellar tendon injury among volleyball players,” Journal of science and medicine in sport / Sports Medicine Australia 9, no. 4 (2006), doi:10.1016/j.jsams.2006.03.015
[16] Wolf Petersen et al., “Patellofemoral pain syndrome,” Knee surgery, sports traumatology, arthroscopy official journal of the ESSKA 22, no. 10 (2014), doi:10.1007/s00167-013-2759-6
[17] Kerry J. Mann et al., “A lower limb assessment tool for athletes at risk of developing patellar tendinopathy,” Medicine and science in sports and exercise 45, no. 3 (2013), doi:10.1249/MSS.0b013e318275e0f2
[18] Petersen et al.
[19] Jodi Aderem and Quinette A. Louw, “Biomechanical risk factors associated with iliotibial band syndrome in runners: a systematic review,” BMC musculoskeletal disorders 16 (2015), doi:10.1186/s12891-015-0808-7
[20] Farzin Halabchi, Reza Mazaheri, and Tohid Seif-Barghi, “Patellofemoral pain syndrome and modifiable intrinsic risk factors; how to assess and address?,” Asian journal of sports medicine 4, no. 2 (2013)
[21] Ibid.
[22] Mann et al.
[23] E. Witvrouw et al., “Intrinsic risk factors for the development of patellar tendinitis in an athletic population. A two-year prospective study,” The American journal of sports medicine 29, no. 2 (2001)
[24] Petersen et al.
[25] R. W. Bisseling et al., “Relationship between landing strategy and patellar tendinopathy in volleyball,” British Journal of Sports Medicine 41, no. 7 (2007), doi:10.1136/bjsm.2006.032565
[26] Petersen et al.
[27] S. Grau et al., “What are causes and treatment strategies for patellar-tendinopathy in female runners?,” Journal of biomechanics 41, no. 9 (2008), doi:10.1016/j.jbiomech.2008.03.005
[28] Kelly Starrett and Glen Cordoza, Becoming a Supple Leopard: The Ultimate Guide to Resolving Pain, Preventing Injury, and Optimizing Athletic Performance (Tuttle Publishing, 2013), 86
[29] Ibid., 92f
[30] Seyit Citaker et al., “Static balance in patients with patellofemoral pain syndrome,” Sports health 3, no. 6 (2011), doi:10.1177/1941738111420803
[31] A. Frohm et al., “Eccentric treatment for patellar tendinopathy: a prospective randomised short-term pilot study of two rehabilitation protocols,” British Journal of Sports Medicine 41, no. 7 (2007), doi:10.1136/bjsm.2006.032599
[32] Martin Hägglund, Johannes Zwerver, and Jan Ekstrand, “Epidemiology of patellar tendinopathy in elite male soccer players,” The American journal of sports medicine 39, no. 9 (2011), doi:10.1177/0363546511408877
[33] Grau et al.
[34] Heidari
[35] Ibid.
[36] Nienke E. Lankhorst, Bierma-Zeinstra, Sita M A, and Marienke van Middelkoop, “Risk factors for patellofemoral pain syndrome: a systematic review,” The Journal of orthopaedic and sports physical therapy 42, no. 2 (2012), doi:10.2519/jospt.2012.3803
[37] K. M. Khan et al., “Patellar tendinopathy: some aspects of basic science and clinical management,” British journal of sports medicine 32, no. 4 (1998): 351
[38] Håvard Visnes and Roald Bahr, “The evolution of eccentric training as treatment for patellar tendinopathy (jumper’s knee): a critical review of exercise programmes,” British journal of sports medicine 41, no. 4 (2007), doi:10.1136/bjsm.2006.032417
[39] Larry E. Miller and Daniel L. Latt, “Chronic Plantar Fasciitis is Mediated by Local Hemodynamics: Implications for Emerging Therapies,” North American journal of medical sciences 7, no. 1 (2015), doi:10.4103/1947-2714.150080
[40] Mohammad A. Tahririan et al., “Plantar fasciitis,” Journal of research in medical sciences the official journal of Isfahan University of Medical Sciences 17, no. 8 (2012)
[41] Brett D. Owens et al., “Risk Factors for Lower Extremity Tendinopathies in Military Personnel,” Orthopaedic journal of sports medicine 1, no. 1 (2013), doi:10.1177/2325967113492707
[42] Jonathan M. Labovitz, Jenny Yu, and Chul Kim, “The role of hamstring tightness in plantar fasciitis,” Foot & ankle specialist 4, no. 3 (2011), doi:10.1177/1938640010397341
[43] Tahririan et al.
[44] Miller and Latt
[45] Tae Im Yi et al., “Clinical characteristics of the causes of plantar heel pain,” Annals of rehabilitation medicine 35, no. 4 (2011), doi:10.5535/arm.2011.35.4.507
[46] Tahririan et al.
[47] Miller and Latt
[48] Karl B. Landorf, Anne-Maree Keenan, and Robert D. Herbert, “Effectiveness of foot orthoses to treat plantar fasciitis: a randomized trial,” Archives of internal medicine 166, no. 12 (2006), doi:10.1001/archinte.166.12.1305
[49] Robert A. Werner et al., “Risk factors for plantar fasciitis among assembly plant workers,” PM & R the journal of injury, function, and rehabilitation 2, no. 2 (2010), doi:10.1016/j.pmrj.2009.11.012
[50] Konstantinos Fousekis, Elias Tsepis, and George Vagenas, “Intrinsic risk factors of noncontact ankle sprains in soccer: a prospective study on 100 professional players,” The American Journal of Sports Medicine 40, no. 8 (2012), doi:10.1177/0363546512449602
[51] G. D. McKay, “Ankle injuries in basketball: injury rate and risk factors,” British Journal of Sports Medicine 35, no. 2 (2001), doi:10.1136/bjsm.35.2.103
[52] Bruce D. Beynnon, Darlene F. Murphy, and Denise M. Alosa, “Predictive Factors for Lateral Ankle Sprains: A Literature Review,” Journal of athletic training 37, no. 4 (2002)
[53] A. K. Ramanathan et al., “The influence of shoe sole’s varying thickness on lower limb muscle activity,” Foot and ankle surgery official journal of the European Society of Foot and Ankle Surgeons 17, no. 4 (2011), doi:10.1016/j.fas.2010.07.003
[54] Cary Groner, “Ankle sprain prevention revisits shoes as solution,” Lower Extremity Review, accessed March 13, 2016, http://lermagazine.com/article/ankle-sprain-prevention-revisits-shoes-as-solution
[55] Fousekis, Tsepis and Vagenas
[56] Beynnon, Murphy and Alosa
[57] You-Jou Hung, “Neuromuscular control and rehabilitation of the unstable ankle,” World journal of orthopedics 6, no. 5 (2015), doi:10.5312/wjo.v6.i5.434
[58] Tine M. Willems et al., “Intrinsic risk factors for inversion ankle sprains in male subjects: a prospective study,” The American Journal of Sports Medicine 33, no. 3 (2005)
[59] Dario Riva et al., “Proprioceptive Training and Injury Prevention in a Professional Men’s Basketball Team: A Six-Year Prospective Study,” Journal of strength and conditioning research / National Strength & Conditioning Association 30, no. 2 (2016), doi:10.1519/JSC.0000000000001097
[60] Beynnon, Murphy and Alosa
[61] Hung
[62] Riva et al.
[63] R. Bahr, O. Lian, and I. A. Bahr, “A twofold reduction in the incidence of acute ankle sprains in volleyball after the introduction of an injury prevention program: a prospective cohort study,” Scandinavian journal of medicine & science in sports 7, no. 3 (1997)
[64] Brett M. Andres and George A. C. Murrell, “Treatment of tendinopathy: what works, what does not, and what is on the horizon,” Clinical orthopaedics and related research 466, no. 7 (2008), doi:10.1007/s11999-008-0260-1
[65] Maria E. H. Larsson, Ingela Käll, and Katarina Nilsson-Helander, “Treatment of patellar tendinopathy—a systematic review of randomized controlled trials,” Knee Surgery, Sports Traumatology, Arthroscopy 20, no. 8 (2012): 1645, doi:10.1007/s00167-011-1825-1
[66] Reed Ferber, Karen D. Kendall, and Lindsay Farr, “Changes in knee biomechanics after a hip-abductor strengthening protocol for runners with patellofemoral pain syndrome,” Journal of athletic training 46, no. 2 (2011), doi:10.4085/1062-6050-46.2.142
[67] Thiago Y. Fukuda et al., “Hip posterolateral musculature strengthening in sedentary women with patellofemoral pain syndrome: a randomized controlled clinical trial with 1-year follow-up,” The Journal of orthopaedic and sports physical therapy 42, no. 10 (2012), doi:10.2519/jospt.2012.4184
[68] Nienke E. Lankhorst, Sita M. A. Bierma-Zeinstra, and Marienke van Middelkoop, “Factors associated with patellofemoral pain syndrome: a systematic review,” British journal of sports medicine, 2012, doi:10.1136/bjsports-2011-090369
[69] Eduardo Magalhães et al., “ISOMETRIC STRENGTH RATIOS OF THE HIP MUSCULATURE IN FEMALES WITH PATELLOFEMORAL PAIN: A COMPARISON TO PAINFREE CONTROLS,” Journal of strength and conditioning research / National Strength & Conditioning Association, 2012, doi:10.1519/JSC.0b013e318279793d
[70] Erik P. Meira and Jason Brumitt, “Influence of the hip on patients with patellofemoral pain syndrome: a systematic review,” Sports health 3, no. 5 (2011), doi:10.1177/1941738111415006
[71] Hossein Negahban et al., “The effects of muscle fatigue on dynamic standing balance in people with and without patellofemoral pain syndrome,” Gait & posture, 2012, doi:10.1016/j.gaitpost.2012.07.025
[72] Christian J. Barton et al., “Gluteal muscle activity and patellofemoral pain syndrome: a systematic review,” British journal of sports medicine, 2012, doi:10.1136/bjsports-2012-090953
[73] Petersen et al.
